Yes, we all are.
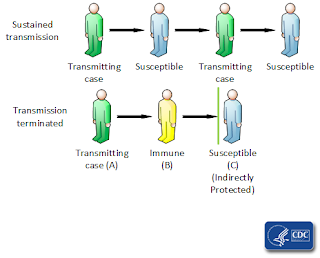
When discussing the spread of infectious diseases, it is useful to understand the concept of “herd immunity.” Infectious diseases spread from individual to individual within the population (or herd). The more individuals a person in the infectious stage of a disease contacts, the more quickly the disease spreads throughout the population. Isolation, quarantine, and physical distancing strategies are all ways to curtail this spread.
So is immunization. We tend to think of immunization as protection for the inoculated individual, and it does indeed do that. But it also protects others in the population. Individuals who have become immune to a disease, whether by vaccination or by contracting the disease and recovering from it, can no longer infect others. By reducing the number of persons who can spread a disease, the progression of it through the population is slowed or halted. Individuals who are not immune are less likely to contact a person who can infect them. This is the basis of herd immunity.
 |
| CDC graphic explaining herd immunity |
Herd immunity does not mean that every individual in the population is immune to the pathogen. In fact, some individuals may not be able to become immune, due to immunodeficiency or immunosuppression. The best way to protect these individuals is through herd immunity, by making it less likely that they would come in contact with someone who is infectious.
Some important things to remember about herd immunity include that it is specific to a particular pathogen, and that it takes time to develop. The length of time required will vary by location and by characteristics of the pathogen. A higher level of immunity among the population is required to establish herd immunity from highly contagious diseases. Those individuals who are immune can come out of isolation and begin to go about their normal daily activities without fear of either contracting the disease or passing it along to others.